Fibromyalgia: what is it and what are the early symptoms?
Fibromyalgia is a rheumatic disease that affects the musculo-skeletal apparatus and consists in chronic widespread pain, stiff and aching muscles, tendons and joints. 90% of patients suffering from this disease also experience chronic fatigue and sleep disturbance.
To date, little is still known of fibromyalgia, above all with regard to the causes. Diagnosis is also difficult, as there are no specific tests able to identify this syndrome with certainty. For this very reason it is important to learn to recognise the early signs and what to do to limit as far as possible any worsening of symptoms and the course of the disease, which over time can risk becoming a debilitating condition.
What is Fibromyalgia and who is most at risk?
Fibromyalgia syndrome is considered a systemic problem that involves biochemical, neuroendocrine and physiological disorders, and leads to a disturbance in the processing and perception of pain. In the cases of serious fibromyalgia, this can cause allodynia, in other words a painful sensation following a normally innocuous stimulus (such as combing hair, pressing slightly on the skin, contact of an object with the body) or hyperalgesia, i.e. hypersensitivity to painful stimuli with consequent lowering of the pain threshold.
As we will see in this article, Fibromyalgia is a highly complex syndrome involving numerous factors, which can have a serious impact and significantly disrupt daily life. This syndrome mainly affects women (around 90% of cases) and symptoms appear at a young age, typically aged between 25 and 55.
Are there specific causes attributable to Fibromyalgia?
The actual cause leading to the development of Fibromyalgia has still not been clarified, but scientific studies suggest that it stems from a malfunction of the Central Nervous System characterized by central sensitisation, which is a heightened pain perception accompanied by ineffective pain inhibition and/or modulation.
This increased response to peripheral stimuli causes often debilitating symptoms, such as hyperalgesia (a stimulus that is more painful than normal), allodynia (a normally painless stimulus that however causes pain) and referred pain across multiple spinal segments, resulting in chronic widespread pain.
Unfortunately, fibromyalgic syndrome tends to degenerate over time, triggering a series of disorders in the neurological, immune, endocrinological and enteric systems.
The early symptoms of Fibromyalgia
The main symptom of Fibromyalgia is muscle pain, often described by patients as intense or burning pain, regardless of the physical activity performed. In addition to this, patients often suffer from asthenia, i.e. chronic fatigue, both physical and mental, as well as the presence of the so-called Tender Points, contracted muscle areas that are painful to touch.
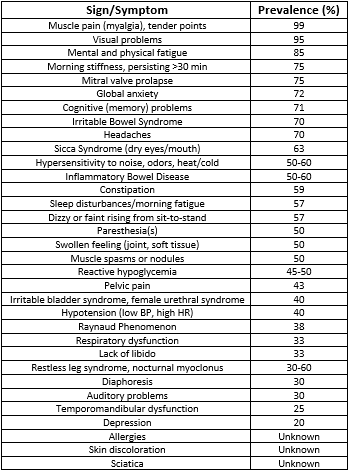 Figure 1: Symptoms of Fibromyalgia – Fonte Physio-Pedia.com
Figure 1: Symptoms of Fibromyalgia – Fonte Physio-Pedia.com
Symptoms of Fibromyalgia, in most cases, are exacerbated by:
- Stress
- Overloading physical activity
- Damp or chilly weather
Those suffering from Fibromyalgia are also likely to present with a number of co-morbidities, in particular:
- Sleep disturbances
- Depression
- Anxiety
- Rheumatoid Arthritis (RA)
- Lupus
- Ankylosing spondylitis (AS)
How to recognise the early symptoms of Fibromyalgia and who to see
If you suffer from chronic widespread pain in various areas of the body, which don’t improve with physiotherapy, combined with a very low tolerance of physical exercise and constant fatigue, this may be Fibromyalgia. However, to get the correct diagnosis and start targeted treatment, it is essential to seek advice from a doctor specialised in Rheumatology or Orthpaedics.
Diagnosis
There is currently no diagnostic test to determine the condition of Fibromyalgia. The diagnosis is usually made by the doctor on the basis of results of a physical examination and excluding other similar conditions.
No specific laboratory or radiology tests are necessary, but a laboratory test may be recommended to exclude other conditions. A diagnosis of Fibromyalgia in fact does not exclude the presence of other clinically significant illnesses. These tests include: Full blood count, VES, standard biochemistry, thyroid levels (TSH, T3 and T4) and rheumatoid factor.
To date, Fibromyalgia is diagnosed when all the following criteria are met:
- Widespread Pain Index (WPI) ≥7 and Symptom Severity Scale (SSS) ≥5; or WPI 4–6 and SSS ≥9.
- Generalised pain is present, defined in at least 4 out of 5 regions.
- Symptoms have been present at a similar level for at least 3 months.
From the patient’s psychological point of view it is important to reach a diagnosis, because often those suffering from chronic widespread pain are unable to find an explanation and consequently a valid treatment for managing the symptoms.
Is there are cure for Fibromyalgia?
There is currently no definitive cure for Fibromyalgia. However, it is important for those with this syndrome to find the best way of managing the syndrome and learning to live with it, limiting as far as possible the impact of symptoms on daily life, which in more serious cases can make this syndrome an effectively seriously debilitating condition.
The treatment of fibromyalgia must be multidisciplinary and personalised according to the response of the individual patient, but generally includes:
- Pharmacological treatments to help control symptoms;
- Education of the patient on the syndrome, to enable the best way to independently manage symptoms;
- Light and supervised physical activity;
- Relaxation techniques such as meditation, breathing techniques, etc.;
- Light massage therapy, manual lymphatic and drainage techniques;
- Change in nutrition, supervised by a nutritionist;
- Water gymnastics, ideally in a heated pool;
- Psychological or Psychotherapy support;
- Other techniques such as acupuncture, osteopathy, occupational therapy, etc.
Could physiotherapy be useful to alleviate the symptoms of Fibromyalgia?
In the case of Fibromyalgia, physiotherapy, in the same way as osteopathy or massages, has a purely symptomatic purpose, in other words, that of alleviating the pain. Based on the experience of our physiotherapists, treatments may be useful, but must be with a “soft” approach, spacing sessions with sufficient time intervals between one and the next to enable tissues to recover.
Physical exercise is also useful, provided that it is supervised by the physiotherapist or graduate in Sports Sciences. In particular, to alternate between light aerobics (walking, cycling) and postural and mild muscle strengthening exercises, can help reinforce the musculo-skeletal structures. Also, in this case it is essential to leave sufficient time for recovery between one session and the next, to avoid fatigue and consequent worsening of pain.








